Is your practice application approaching sunset? Are you looking to purchase a new system? Have you recently merged with another group and now have disparate systems that need to be consolidated?
Regardless of your scenario, whether voluntary or involuntary, physicians, practice owners, and healthcare information systems teams must establish an appropriate change management strategy to accomplish a successful transition.
Today, the top drivers for replacing a practice management system include the need for hospital- integrated systems, compliance with state and federal regulations, mergers and acquisitions, cost, data management, patient, and provider satisfaction.
What is the future of your practice? Why are you transitioning?
Before your project begins, it is paramount to have a solid change management plan.
- Identify an executive and a physician level sponsor who will remain committed throughout the project. Provide education on sponsor responsibilities and visibility; this is crucial for success.
- Assemble a cohesive, well balanced team capable of managing effective change. Team members need to understand the practice value and scope of change. They must be comfortable communicating, planning activities to mitigate resistance, and coaching others to embrace the planned change.
An effective change management strategy includes considerations for business processes, the technology, and for all users of the system. Special attention must be paid to both business operations users and the various clinical groups that will rely on the system to enhance patient care.
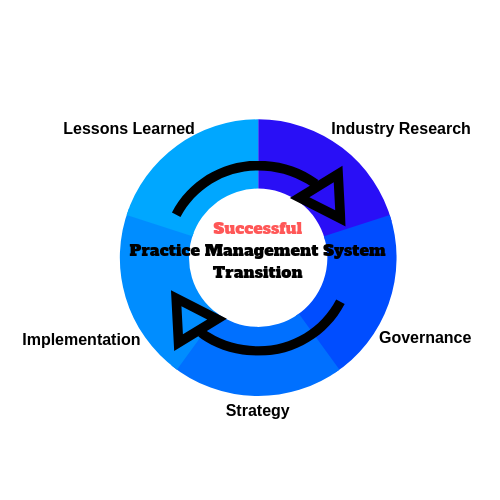
Here are 5 Focus Areas That Drive Successful System Transitions
1. Research Industry
To ensure your practice is compliant with industry standards, examine your current internal operations and identify your future business needs. Utilize MGMA industry benchmark reports to compare and prioritize your practice goals.
Today, value-based patient care models are at the forefront of healthcare. This increases the need to demonstrate practice efficiency and quality care for service reimbursement. Fully integrated systems will enhance clinical workflows and facilitate quicker reimbursement processing, allowing providers to spend more time at the point of care.
Select a robust practice management system that boasts a unified platform. Examples include systems with secure patient portals, ancillary system integration, revenue cycle management, clinical documentation and decision support.
2. Governance
Governance of the transition is as important as the new application’s functionality. Formalize a governance strategy and identify the key stakeholders who will make or approve policy changes.
A successful application migration can drive greater organizational change and lead to overall physician, staff, and patient satisfaction. Strong governance positions the practice to:
- Continue to meet regulatory guidelines
- Continue to meet quality standards
- Achieve faster adoption and usage rates
- Improve operational efficiency
3. Strategy
Practice groups continue to differ in specialty, services provided, practice structure, population served, practice size, and physical location. Support must be customized and delivered to each practice with consideration for the differentiating elements.
Who is responsible for leading your clinical and revenue cycle workflow discussions?
Consider resources with deep knowledge who add perspective to the process as these specific questions are answered.
- Will new technology enhance workflows and aid your efforts to provide quality patient care?
- Will the new practice management system have similar or new limitations?
- How will the transition impact your clinical and office support staff?
- How will the costs associated with new implementation impact your practice budget?
- What effects will MIPS/ MACRA have on the practice?
- How will compliance and reporting structures change?
- Does the sourced vendor meet your practice needs?
- What are the advantages/ disadvantages to internal vs. remote or cloud storage?
4. Implementation
Early engagement of strong project leadership ensures there is a detailed plan and each step aligns with your leadership and practice goals. Effective communication, careful review of current/ future state, planning, execution, and ongoing project monitoring requires expertise.
Use a systematic approach when managing:
- Data conversion
- Maintenance
- Integrated Testing
- Training
- Go Live
- Post Live
Failure to comply with this recommendation may cause your practice to incur additional project costs. Implementing a new system for your practice is an investment and once your new system is in place, operational excellence and increased ROI are achievable.
Have you identified who will lead your implementation?
5. Lessons Learned
Due to the complex nature of a system transition, leveraging proven methodologies adds value to the process. Lessons learned from larger, inpatient entities can be scaled to meet individual practice needs. Understanding project management, communication, and risk identification allows for better planning, measurement of value achieved, and project success.
What lessons have your team members learned from other system implementations?
How can your practice plan for issues with diagnostic or device interfaces, chart abstraction, or choosing an effective training methodology?
Where are you in the process? Have you thoroughly considered?
- Search & Selection
- Data Warehousing
- New Implementation
- Application or Legacy Support
- Post Sunset Support





